Letters to Baby While in Waiting Room During Labor
This article is about birth in humans. For birth in other mammals, see Birth.
Expulsion of a fetus from the pregnant mother's uterus
Medical condition
| Childbirth | |
|---|---|
| Other names | Labour and delivery, labor and delivery, partus, giving birth, parturition, birth, confinement[1] [2] |
 | |
| Newborn baby and mother with vernix covering on the baby | |
| Specialty | Obstetrics, midwifery |
| Complications | Obstructed labour, postpartum bleeding, eclampsia, postpartum infection, birth asphyxia, neonatal hypothermia[3] [4] [5] |
| Types | Vaginal delivery, C-section[6] [7] |
| Causes | Pregnancy |
| Prevention | Birth control, elective abortion |
| Frequency | 135 million (2015)[8] |
| Deaths | 500,000 maternal deaths a year[5] |
Childbirth, also known as labour or delivery, is the ending of pregnancy where one or more babies leaves the uterus by passing through the vagina or by Caesarean section.[7] In 2015, there were about 135 million births globally.[8] About 15 million were born before 37 weeks of gestation,[9] while between 3 and 12% were born after 42 weeks.[10] In the developed world most deliveries occur in hospitals,[11] [12] while in the developing world most births take place at home with the support of a traditional birth attendant.[13]
The most common way of childbirth is a vaginal delivery.[6] It involves three stages of labour: the shortening and opening of the cervix during the first stage, descent and birth of the baby during the second stage, and the delivery of the placenta during the third stage.[14] [15] The first stage begins with crampy abdominal or back pain that lasts around half a minute and occurs every 10 to 30 minutes.[14] The pain becomes stronger and closer together over time.[15] The second stage ends when the infant is fully expelled. In the third stage, the delivery of the placenta, delayed clamping of the umbilical cord is generally recommended.[16] As of 2014,[update] all major health organisations advise that immediately following vaginal birth, or as soon as the mother is alert and responsive after a Caesarean section, that the infant be placed on the mother's chest, termed skin-to-skin contact, delaying routine procedures for at least one to two hours or until the baby has had its first breastfeeding.[17] [18] [19]
Most babies are born head first; however about 4% are born feet or buttocks first, known as breech.[15] [20] Typically the head enters the pelvis facing to one side, and then rotates to face down.[21] During labour, the woman giving birth can generally eat and move around as they like.[22] A number of methods can help with pain, such as relaxation techniques, opioids, and spinal blocks.[15] While making a cut to the opening of the vagina, known as an episiotomy, is common, it is generally not needed.[15] In 2012, about 23 million deliveries occurred by Caesarean section, an operation on the abdomen.[23] [15]
Each year, complications from pregnancy and childbirth result in about 500,000 birthing deaths, seven million women have serious long-term problems, and 50 million women giving birth have negative health outcomes following delivery.[5] Most of these occur in the developing world.[5] Specific complications include obstructed labour, postpartum bleeding, eclampsia, and postpartum infection.[5] Complications in the baby may include lack of oxygen at birth, birth trauma, prematurity, and infections.[4] [24]
Signs and symptoms [edit]

The most prominent sign of labour is strong repetitive uterine contractions. The distress levels reported by labouring woman vary widely. They appear to be influenced by fear and anxiety levels, experience with prior childbirth, cultural ideas of childbirth pain, mobility during labour, and the support received during labour.[25] [26] Personal expectations, the amount of support from caregivers, quality of the caregiver-patient relationship, and involvement in decision-making are more important in mother's overall satisfaction with the experience of childbirth than are other factors such as age, socioeconomic status, ethnicity, preparation, physical environment, pain, immobility, or medical interventions.[27]
Descriptions [edit]
Pain in contractions has been described as feeling similar to very strong menstrual cramps. Women giving birth are often encouraged to refrain from screaming. However, moaning and grunting may be encouraged to help lessen pain. Crowning may be experienced as an intense stretching and burning. Even those who show little reaction to labour pains, in comparison to others, show a substantially severe reaction to crowning (the appearance of the baby's head).[ citation needed ]
Back labour is a term for specific pain occurring in the lower back, just above the tailbone, during childbirth.[28]
Psychological [edit]
During the later stages of gestation there is an increase in abundance of oxytocin, a hormone that is known to evoke feelings of contentment, reductions in anxiety, and feelings of calmness and security around the mate.[29] Oxytocin is further released during labour when the fetus stimulates the cervix and vagina, and it is believed that it plays a major role in the bonding of a birther to their infant and in the establishment of "maternal" behaviour. The act of nursing a child also causes a release of oxytocin.[30]
Between 70% and 80% of woman who give birth in the United States report some feelings of sadness or "baby blues" after giving birth.[ medical citation needed ] The symptoms normally occur for a few minutes up to few hours each day and they should lessen and disappear within two weeks after delivery. Postpartum depression may develop in some women. Preventive group therapy has proven effective as a prophylactic treatment for postpartum depression.[ medical citation needed ] [31] [32]
Vaginal birth [edit]
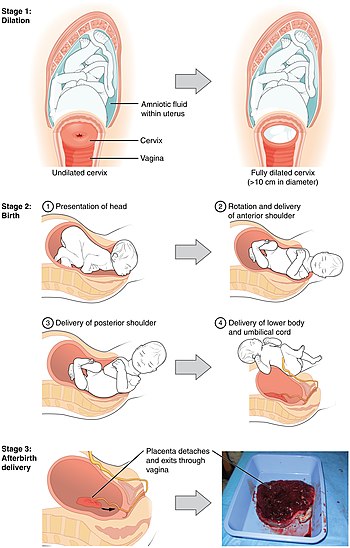
Sequence of images showing the stages of ordinary childbirth
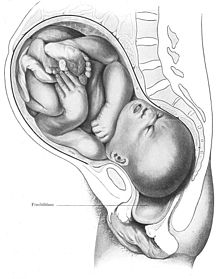
Humans are bipedal with an erect stance. The erect posture causes the weight of the abdominal contents to thrust on the pelvic floor, a complex structure which must not only support this weight but allow, in women, three channels to pass through it: the urethra, the vagina and the rectum. The infant's head and shoulders must go through a specific sequence of manoeuvres in order to pass through the ring of the mother's pelvis.
Six phases of a typical vertex or cephalic (head-first presentation) delivery:
- Engagement of the fetal head in the transverse position. The baby's head is facing across the pelvis at one or other of the mother's hips.
- Descent and flexion of the fetal head.
- Internal rotation. The fetal head rotates 90 degrees to the occipito-anterior position so that the baby's face is towards the mother's rectum.
- Delivery by extension. The fetal head is bowed, chin on chest, so that the back or crown of its head leads the way through the birth canal, until the back of its neck presses against the pubic bone and its chin leaves its chest, extending the neck – as if to look up, and the rest of its head passes out of the birth canal.
- Restitution. The fetal head turns through 45 degrees to restore its normal relationship with the shoulders, which are still at an angle.
- External rotation. The shoulders repeat the corkscrew movements of the head, which can be seen in the final movements of the fetal head.
The vagina is called a 'birth canal' when the baby enters this passage.
Station refers to the relationship of the fetal presenting part to the level of the ischial spines. When the presenting part is at the ischial spines the station is 0 (synonymous with engagement). If the presenting fetal part is above the spines, the distance is measured and described as minus stations, which range from −1 to −4 cm. If the presenting part is below the ischial spines, the distance is stated as plus stations ( +1 to +4 cm). At +3 and +4 the presenting part is at the perineum and can be seen.[33]
The fetal head may temporarily change shape substantially (becoming more elongated) as it moves through the birth canal. This change in the shape of the fetal head is called molding and is much more prominent in women having their first vaginal delivery.[34]
Cervical ripening is the physical and chemical changes in the cervix to prepare it for the stretching that will take place as the fetus moves out of the uterus and into the birth canal. A scoring system called a Bishop score can be used to judge the degree of cervical ripening in order to predict the timing of labour and delivery of the infant or for women at risk for preterm labour. It is also used to judge when a woman will respond to induction of labour for a postdate pregnancy or other medical reasons. There are several methods of inducing cervical ripening which will allow the uterine contractions to effectively dilate the cervix.[35]
Onset of labour [edit]

The hormones initiating labour
Definitions of the onset of labour include:
- Regular uterine contractions at least every six minutes with evidence of change in cervical dilation or cervical effacement between consecutive digital examinations.[36]
- Regular contractions occurring less than 10 minutes apart and progressive cervical dilation or cervical effacement.[37]
- At least three painful regular uterine contractions during a 10-minute period, each lasting more than 45 seconds.[38]
Many women are known to experience what has been termed the "nesting instinct". Women report a spurt of energy shortly before going into labour.[39] Common signs that labour is about to begin may include what is known as lightening, which is the process of the baby moving down from the rib cage with the head of the baby engaging deep in the pelvis. The pregnant woman may then find breathing easier, since her lungs have more room for expansion, but pressure on her bladder may cause more frequent need to void (urinate). Lightening may occur a few weeks or a few hours before labour begins, or even not until labour has begun.[39] Some women also experience an increase in vaginal discharge several days before labour begins when the "mucus plug", a thick plug of mucus that blocks the opening to the uterus, is pushed out into the vagina. The mucus plug may become dislodged days before labour begins or not until the start of labour.[39]
While inside the uterus the baby is enclosed in a fluid-filled membrane called the amniotic sac. Shortly before, at the beginning of, or during labour the sac ruptures. Once the sac ruptures, termed "the water breaks", the baby is at risk for infection and the mother's medical team will assess the need to induce labour if it has not started within the time they believe to be safe for the infant.[39]

Folklore has long held that most babies are born in the late night or very early morning; 2018 research has found this to be correct in the US, but only for babies born at home or on Saturday or Sunday. All other births are most likely to occur between 8 a.m. and noon, a reflection of the fact that planned C-sections are generally scheduled for 8 a.m. Likewise, births from induced deliveries rise during the morning hours and peak at 3 p.m. The most likely day of the week for a baby's birth in the US is Monday, followed by Tuesday, likely related to scheduled deliveries as well.[ better source needed ] [40] [41]
The first stage of labour is divided into latent and active phases, where the latent phase is sometimes included in the definition of labour,[42] and sometimes not.[43]
First stage: latent phase [edit]
The latent phase is generally defined as beginning at the point at which the woman perceives regular uterine contractions.[44] In contrast, Braxton Hicks contractions, which are contractions that may start around 26 weeks gestation and are sometimes called "false labour", are infrequent, irregular, and involve only mild cramping.[45]
Cervical effacement, which is the thinning and stretching of the cervix, and cervical dilation occur during the closing weeks of pregnancy. Effacement is usually complete or near-complete and dilation is about 5 cm by the end of the latent phase.[46] The degree of cervical effacement and dilation may be felt during a vaginal examination. The latent phase ends with the onset of the active first stage.
First stage: active phase [edit]
Engagement of the fetal head
The active stage of labour (or "active phase of first stage" if the previous phase is termed "latent phase of first stage") has geographically differing definitions. The World Health Organization describes the active first stage as "a period of time characterised by regular painful uterine contractions, a substantial degree of cervical effacement and more rapid cervical dilatation from 5 cm until full dilatation for first and subsequent labours.[47] In the US, the definition of active labour was changed from 3 to 4 cm, to 5 cm of cervical dilation for multiparous women, mothers who had given birth previously, and at 6 cm for nulliparous women, those who had not given birth before.[48] This was done in an effort to increase the rates of vaginal delivery.[49]
Health care providers may assess a labouring mother's progress in labour by performing a cervical exam to evaluate the cervical dilation, effacement, and station. These factors form the Bishop score. The Bishop score can also be used as a means to predict the success of an induction of labour.
During effacement, the cervix becomes incorporated into the lower segment of the uterus. During a contraction, uterine muscles contract causing shortening of the upper segment and drawing upwards of the lower segment, in a gradual expulsive motion.[50] The presenting fetal part then is permitted to descend. Full dilation is reached when the cervix has widened enough to allow passage of the baby's head, around 10 cm dilation for a term baby.
A standard duration of the latent first stage has not been established and can vary widely from one woman to another. However, the duration of active first stage (from 5 cm until full cervical dilatation) usually does not extend beyond 12 hours in first labours ("primiparae"), and usually does not extend beyond 10 hours in subsequent labours ("multiparae").[51]
Dystocia of labour, also called "dysfunctional labour" or "failure to progress", is difficult labour or abnormally slow progress of labour, involving progressive cervical dilatation or lack of descent of the fetus. Friedman's Curve, developed in 1955, was for many years used to determine labour dystocia. However, more recent medical research suggests that the Friedman curve may not be currently[ when? ] applicable.[52] [53]
Second stage: fetal expulsion [edit]

Stages in the birth of the baby's head

The expulsion stage begins when the cervix is fully dilated, and ends when the baby is born. As pressure on the cervix increases, a sensation of pelvic pressure is experienced, and, with it, an urge to begin pushing. At the beginning of the normal second stage, the head is fully engaged in the pelvis; the widest diameter of the head has passed below the level of the pelvic inlet. The fetal head then continues descent into the pelvis, below the pubic arch and out through the vaginal introitus (opening). This is assisted by the additional maternal efforts of "bearing down" or pushing, similar to defecation. The appearance of the fetal head at the vaginal orifice is termed the "crowning". At this point, the mother will feel an intense burning or stinging sensation.
When the amniotic sac has not ruptured during labour or pushing, the infant can be born with the membranes intact. This is referred to as "delivery en caul".
Complete expulsion of the baby signals the successful completion of the second stage of labour. Some babies, especially preterm infants, are born covered with a waxy or cheese-like white substance called vernix. It is thought to have some protective roles during fetal development and for a few hours after birth.
The second stage varies from one woman to another. In first labours, birth is usually completed within three hours whereas in subsequent labours, birth is usually completed within two hours.[54] Second-stage labours longer than three hours are associated with declining rates of spontaneous vaginal delivery and increasing rates of infection, perineal tears, and obstetric haemorrhage, as well as the need for intensive care of the neonate.[55]
Third stage: placenta delivery [edit]
The period from just after the fetus is expelled until just after the placenta is expelled is called the third stage of labour or the involution stage. Placental expulsion begins as a physiological separation from the wall of the uterus. The average time from delivery of the baby until complete expulsion of the placenta is estimated to be 10–12 minutes dependent on whether active or expectant management is employed.[56] In as many as 3% of all vaginal deliveries, the duration of the third stage is longer than 30 minutes and raises concern for retained placenta.[57]
Placental expulsion can be managed actively or it can be managed expectantly, allowing the placenta to be expelled without medical assistance. Active management is the administration of a uterotonic drug within one minute of fetal delivery, controlled traction of the umbilical cord and fundal massage after delivery of the placenta, followed by performance of uterine massage every 15 minutes for two hours.[58] In a joint statement, World Health Organization, the International Federation of Gynaecology and Obstetrics and the International Confederation of Midwives recommend active management of the third stage of labour in all vaginal deliveries to help to prevent postpartum haemorrhage.[59] [60] [61]
Delaying the clamping of the umbilical cord for at least one minute or until it ceases to pulsate, which may take several minutes, improves outcomes as long as there is the ability to treat jaundice if it occurs. For many years it was believed that late cord cutting led to a mother's risk of experiencing significant bleeding after giving birth, called postpartum bleeding. However a recent review found that delayed cord cutting in healthy full-term infants resulted in early haemoglobin concentration and higher birthweight and increased iron reserves up to six months after birth with no change in the rate of postpartum bleeding.[62] [63]
Fourth stage [edit]

Newborn rests as caregiver checks breath sounds
The "fourth stage of labour" is the period beginning immediately after the birth of a child and extending for about six weeks. The terms postpartum and postnatal are often used for this period.[64] The woman's body, including hormone levels and uterus size, return to a non-pregnant state and the newborn adjusts to life outside the mother's body. The World Health Organization (WHO) describes the postnatal period as the most critical and yet the most neglected phase in the lives of mothers and babies; most deaths occur during the postnatal period.[65]
Following the birth, if the mother had an episiotomy or a tearing of the perineum, it is stitched. This is also an optimal time for uptake of long-acting reversible contraception (LARC), such as the contraceptive implant or intrauterine device (IUD), both of which can be inserted immediately after delivery while the woman is still in the delivery room.[66] [67] The mother has regular assessments for uterine contraction and fundal height,[68] vaginal bleeding, heart rate and blood pressure, and temperature, for the first 24 hours after birth. The first passing of urine should be documented within six hours.[65] Afterpains (pains similar to menstrual cramps), contractions of the uterus to prevent excessive blood flow, continue for several days. Vaginal discharge, termed "lochia", can be expected to continue for several weeks; initially bright red, it gradually becomes pink, changing to brown, and finally to yellow or white.[69] Some women experience an uncontrolled episode of shivering or postpartum chills, after the birth.[ citation needed ]
Until recently[ when? ] babies born in hospitals were removed from their mothers shortly after birth and brought to the mother only at feeding times. Mothers were told that their newborn would be safer in the nursery and that the separation would offer the mother more time to rest. As attitudes began to change, some hospitals offered a "rooming in" option wherein after a period of routine hospital procedures and observation, the infant could be allowed to share the mother's room. As of 2020, rooming in has increasingly become standard practice in maternity wards.[70]
Around 2000[ dubious – discuss ] [ citation needed ] authorities began to question the practice of removing the newborn immediately postpartum for routine postnatal procedures before being returned to the mother. Some authorities began to suggest that early skin-to-skin contact (placing the naked baby on the mother's chest) may benefit both mother and infant. Using animal studies that showed that the intimate contact inherent in skin-to-skin contact promotes neurobehaviors that result in the fulfilment of basic biological needs as a model, studies were done to assess what, if any, advantages may be associated with early skin-to-skin contact for human mothers and their babies. A 2011 medical review found that early skin-to-skin contact, sometimes called kangaroo care, resulted in improved breastfeeding outcomes, cardio-respiratory stability, and a decrease in infant crying.[71] [72] A 2016 Cochrane review found that skin-to-skin contact at birth promotes the likelihood and effectiveness of breastfeeding.[73]
As of 2014, early postpartum skin-to-skin contact is endorsed by all major organisations that are responsible for the well-being of infants, including the American Academy of Pediatrics.[17] The World Health Organization (WHO) states that "the process of childbirth is not finished until the baby has safely transferred from placental to mammary nutrition." It is advised that the newborn be placed skin-to-skin with the mother following vaginal birth, or as soon as the mother is alert and responsive after a Caesarean section, postponing any routine procedures for at least one to two hours. The WHO suggests that any initial observations of the infant can be done while the infant remains close to the mother, saying that even a brief separation before the baby has had its first feed can disturb the bonding process. They further advise frequent skin-to-skin contact as much as possible during the first days after delivery, especially if it was interrupted for some reason after the delivery.[18] [19]
Labour induction and elective Caesarean section [edit]
In many cases and with increasing frequency, childbirth is achieved through labour induction or caesarean section. Labour induction is the process or treatment that stimulates childbirth and delivery. Inducing labour can be accomplished with pharmaceutical or non-pharmaceutical methods. Inductions are most often performed either with prostaglandin drug treatment alone, or with a combination of prostaglandin and intravenous oxytocin treatment.[74] Caesarean section is the removal of the neonate through a surgical incision in the abdomen, rather than through vaginal birth.[75] Childbirth by C-Sections increased 50% in the US from 1996 to 2006. In 2011, 32.8 per cent of births in the US were delivered by cesarean section.[75] Induced births and elective cesarean before 39 weeks can be harmful to the neonate as well as harmful or without benefit to the mother. Therefore, many guidelines recommend against non-medically required induced births and elective cesarean before 39 weeks.[76] The 2012 rate of labour induction in the United States was 23.3 per cent, and has more than doubled from 1990 to 2010.[77] [78] The American Congress of Obstetricians and Gynecologists (ACOG) guidelines recommend a full evaluation of the maternal-fetal status, the status of the cervix, and at least a 39 completed weeks (full term) of gestation for optimal health of the newborn when considering elective induction of labour. Per these guidelines, indications for induction may include:
- Abruptio placentae
- Chorioamnionitis
- Fetal compromise such as isoimmunisation leading to haemolytic disease of the newborn or oligohydramnios
- Fetal demise
- Gestational hypertension
- Maternal conditions such as gestational diabetes or chronic kidney disease
- Preeclampsia or eclampsia
- Premature rupture of membranes
- Postterm pregnancy
Induction is also considered for logistical reasons, such as the distance from hospital or psychosocial conditions, but in these instances gestational age confirmation must be done, and the maturity of the fetal lung must be confirmed by testing. The ACOG also note that contraindications for induced labour are the same as for spontaneous vaginal delivery, including vasa previa, complete placenta praevia, umbilical cord prolapse or active genital herpes simplex infection.[79]
Management [edit]
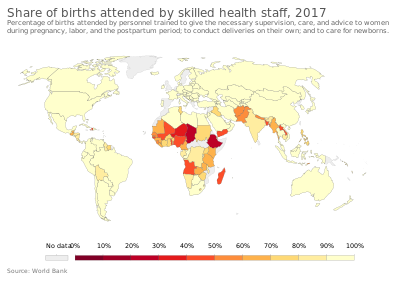
Share of births attended by skilled health staff[80]
Deliveries are assisted by a number of professionals including: obstetricians, family physicians and midwives. For low risk pregnancies all three result in similar outcomes.[81]
Preparation [edit]
Eating or drinking during labour is an area of ongoing debate. While some have argued that eating in labour has no harmful effects on outcomes,[82] others continue to have concern regarding the increased possibility of an aspiration event (choking on recently eaten foods) in the event of an emergency delivery due to the increased relaxation of the oesophagus in pregnancy, upward pressure of the uterus on the stomach, and the possibility of general anaesthetic in the event of an emergency cesarean.[83] A 2013 Cochrane review found that with good obstetrical anaesthesia there is no change in harms from allowing eating and drinking during labour in those who are unlikely to need surgery. They additionally acknowledge that not eating does not mean there is an empty stomach or that its contents are not as acidic. They therefore conclude that "women should be free to eat and drink in labour, or not, as they wish."[84]
At one time shaving of the area around the vagina, was common practice due to the belief that hair removal reduced the risk of infection, made an episiotomy (a surgical cut to enlarge the vaginal entrance) easier, and helped with instrumental deliveries. It is currently less common, though it is still a routine procedure in some countries even though a systematic review found no evidence to recommend shaving.[85] Side effects appear later, including irritation, redness, and multiple superficial scratches from the razor. Another effort to prevent infection has been the use of the antiseptic chlorhexidine or providone-iodine solution in the vagina. Evidence of benefit with chlorhexidine is lacking.[86] A decreased risk is found with providone-iodine when a cesarean section is to be performed.[87]
Forceps or vacuum assisted delivery [edit]
An assisted delivery is used in about 1 in 8 births, and may be needed if either mother or infant appears to be at risk during a vaginal delivery. The methods used are termed obstetrical forceps extraction and vacuum extraction, also called ventouse extraction. Done properly, they are both safe with some preference for forceps rather than vacuum, and both are seen as preferable to an unexpected C-section. While considered safe, some risks for the mother include vaginal tearing, including a higher chance of having a more major vaginal tear that involves the muscle or wall of the anus or rectum. For women undergoing operative vaginal delivery with vacuum extraction or forceps, there is strong evidence that prophylactic antibiotics help to reduce the risk of infection.[88] There is a higher risk of blood clots forming in the legs or pelvis—anti-clot stockings or medication may be ordered to avoid clots. Urinary incontinence is not unusual after childbirth but it is more common after an instrument delivery. Certain exercises and physiotherapy will help the condition to improve.[89]
Pain control [edit]
Non pharmaceutical [edit]
Some women prefer to avoid analgesic medication during childbirth. Psychological preparation may be beneficial. Relaxation techniques, immersion in water, massage, and acupuncture may provide pain relief. Acupuncture and relaxation were found to decrease the number of caesarean sections required.[90] Immersion in water has been found to relieve pain during the first stage of labour and to reduce the need for anaesthesia and shorten the duration of labour, however the safety and efficacy of immersion during birth, water birth, has not been established or associated with maternal or fetal benefit.[91]
Most women like to have someone to support them during labour and birth; such as a midwife, nurse, or doula; or a lay person such as the father of the baby, a family member, or a close friend. Studies have found that continuous support during labour and delivery reduce the need for medication and a caesarean or operative vaginal delivery, and result in an improved Apgar score for the infant.[92] [93]
Pharmaceutical [edit]
Different measures for pain control have varying degrees of success and side effects to the woman and her baby. In some countries of Europe, doctors commonly prescribe inhaled nitrous oxide gas for pain control, especially as 53% nitrous oxide, 47% oxygen, known as Entonox; in the UK, midwives may use this gas without a doctor's prescription.[94] Opioids such as fentanyl may be used, but if given too close to birth there is a risk of respiratory depression in the infant.[ needs update ] [95]
Popular medical pain control in hospitals include the regional anaesthetics epidurals (EDA), and spinal anaesthesia. Epidural analgesia is a generally safe and effective method of relieving pain in labour, but has been associated with longer labour, more operative intervention (particularly instrument delivery), and increases in cost.[96] However, a more recent (2017) Cochrane review suggests that the new epidural techniques have no effect on labour time and the use of instruments or the need for C-section deliveries.[97] Generally, pain and stress hormones rise throughout labour for women without epidurals, while pain, fear, and stress hormones decrease upon administration of epidural analgesia, but rise again later.[98] Medicine administered via epidural can cross the placenta and enter the bloodstream of the fetus.[99] Epidural analgesia has no statistically significant impact on the risk of caesarean section, and does not appear to have an immediate effect on neonatal status as determined by Apgar scores.[97]
Augmentation [edit]

Augmentation is the process of stimulating the uterus to increase the intensity and duration of contractions after labour has begun. Several methods of augmentation are commonly been used to treat slow progress of labour (dystocia) when uterine contractions are assessed to be too weak. Oxytocin is the most common method used to increase the rate of vaginal delivery.[100] The World Health Organization recommends its use either alone or with amniotomy (rupture of the amniotic membrane) but advises that it must be used only after it has been correctly confirmed that labour is not proceeding properly if harm is to be avoided. The WHO does not recommend the use of antispasmodic agents for prevention of delay in labour.[101]
Episiotomy [edit]
For years an episiotomy was thought to help prevent more extensive vaginal tears and heal better than a natural tear. Perineal tears can occur at the vaginal opening as the baby's head passes through, especially if the baby descends quickly. Tears can involve the perineal skin or extend to the muscles and the anal sphincter and anus. Once common, they are now recognised as generally not needed.[15] When needed, the midwife or obstetrician makes a surgical cut in the perineum to prevent severe tears that can be difficult to repair. A 2017 Cochrane review compared episiotomy as needed (restrictive) with routine episiotomy to determine the possible benefits and harms for mother and baby. The review found that restrictive episiotomy policies appeared to give a number of benefits compared with using routine episiotomy. Women experienced less severe perineal trauma, less posterior perineal trauma, less suturing and fewer healing complications at seven days with no difference in occurrence of pain, urinary incontinence, painful sex or severe vaginal/perineal trauma after birth.[102]
Multiple births [edit]
In cases of a head first-presenting first twin, twins can often be delivered vaginally. In some cases twin delivery is done in a larger delivery room or in an operating theatre, in the event of complication e.g.
- Both twins born vaginally – this can occur both presented head first or where one comes head first and the other is breech and/or helped by a forceps/ventouse delivery
- One twin born vaginally and the other by caesarean section.
- If the twins are joined at any part of the body – called conjoined twins, delivery is mostly by caesarean section.
Support [edit]

Baby on warming tray attended to by her father.
Obstetric care frequently subjects women to institutional routines, which may have adverse effects on the progress of labour. Supportive care during labour may involve emotional support, comfort measures, and information and advocacy which may promote the physical process of labour as well as women's feelings of control and competence, thus reducing the need for obstetric intervention. The continuous support may be provided either by hospital staff such as nurses or midwives, doulas, or by companions of the woman's choice from her social network. A 2015 Cochrane review that examined debriefing interventions for women who perceived childbirth as traumatic failed to find any evidence to support routine debriefing as a needed intervention after childbirth.[103] There is increasing evidence to show that the participation of the child's father in the birth leads to better birth and also post-birth outcomes, providing the father does not exhibit excessive anxiety.[ medical citation needed ] [104]
Continuous labour support may help women to give birth spontaneously, that is, without caesarean or vacuum or forceps, with slightly shorter labours, and to have more positive feelings regarding their experience of giving birth. Continuous labour support may also reduce women's use of pain medication during labour and reduce the risk of babies having low five-minute Agpar scores.[105]
Fetal monitoring [edit]
For external monitoring of the fetus during childbirth, a simple pinard stethoscope or doppler fetal monitor ("doptone") can be used. A method of external (noninvasive) fetal monitoring (EFM) during childbirth is cardiotocography (CTG), using a cardiotocograph that consists of two sensors: The heart (cardio) sensor is an ultrasonic sensor, similar to a Doppler fetal monitor, that continuously emits ultrasound and detects motion of the fetal heart by the characteristic of the reflected sound. The pressure-sensitive contraction transducer, called a tocodynamometer (toco) has a flat area that is fixated to the skin by a band around the belly. The pressure required to flatten a section of the wall correlates with the internal pressure, thereby providing an estimate of contraction.[106] Monitoring with a cardiotocograph can either be intermittent or continuous.[107] The World Health Organization (WHO) advises that for healthy women undergoing spontaneous labour continuous cardiotocography is not recommended for assessment of fetal well-being. The WHO states: "In countries and settings where continuous CTG is used defensively to protect against litigation, all stakeholders should be made aware that this practice is not evidence-based and does not improve birth outcomes."[108]
A mother's water has to break before internal (invasive) monitoring can be used. More invasive monitoring can involve a fetal scalp electrode to give an additional measure of fetal heart activity, and/or intrauterine pressure catheter (IUPC). It can also involve fetal scalp pH testing.[ medical citation needed ]
Complications [edit]

Disability-adjusted life year for maternal conditions per 100,000 inhabitants in 2004.[109]
no data
less than 100
100–400
400–800
800–1200
1200–1600
1600–2000
2000–2400
2400–2800
2800–3200
3200–3600
3600–4000
more than 4000

Disability-adjusted life year for perinatal conditions per 100,000 inhabitants in 2004.[109]
no data
less than 100
100–400
400–800
800–1200
1200–1600
1600–2000
2000–2400
2400–2800
2800–3200
3200–3600
3600–4000
more than 4000
Per figures retrieved in 2015, since 1990 there has been a 44 per cent decline in the maternal death rate. However, according to 2015 figures 830 women die every day from causes related to pregnancy or childbirth and for every woman who dies, 20 or 30 encounter injuries, infections or disabilities. Most of these deaths and injuries are preventable.[110] [111]
In 2008, noting that each year more than 100,000 women die of complications of pregnancy and childbirth and at least seven million experience serious health problems while 50 million more have adverse health consequences after childbirth, the World Health Organization (WHO) has urged midwife training to strengthen maternal and newborn health services. To support the upgrading of midwifery skills the WHO established a midwife training program, Action for Safe Motherhood.[5]
The rising maternal death rate in the US is of concern. In 1990 the US ranked 12th of the 14 developed countries that were analysed. However, since that time the rates of every country have steadily continued to improve while the US rate has spiked dramatically. While every other developed nation of the 14 analysed in 1990 shows a 2017 death rate of less than 10 deaths per every 100,000 live births, the US rate has risen to 26.4. By comparison, the United Kingdom ranks second highest at 9.2 and Finland is the safest at 3.8.[112] Furthermore, for every one of the 700 to 900 US woman who die each year during pregnancy or childbirth, 70 experience significant complications such as haemorrhage and organ failure, totalling more than one per cent of all births.[113]
Compared to other developed nations, the United States also has high infant mortality rates. The Trust for America's Health reports that as of 2011, about one-third of American births have some complications; many are directly related to the mother's health including increasing rates of obesity, type 2 diabetes, and physical inactivity. The U.S. Centers for Disease Control and Prevention (CDC) has led an initiative to improve woman's health previous to conception in an effort to improve both neonatal and maternal death rates.[114]
Labour and delivery complications [edit]
Obstructed labour [edit]
The second stage of labour may be delayed or lengthy due to poor or uncoordinated uterine action, an abnormal uterine position such as breech or shoulder dystocia, and cephalopelvic disproportion (a small pelvis or large infant). Prolonged labour may result in maternal exhaustion, fetal distress, and other complications including obstetric fistula.[115]
Eclampsia [edit]
Eclampsia is the onset of seizures (convulsions) in a woman with pre-eclampsia. Pre-eclampsia is a disorder of pregnancy in which there is high blood pressure and either large amounts of protein in the urine or other organ dysfunction. Pre-eclampsia is routinely screened for during prenatal care. Onset may be before, during, or rarely, after delivery. Around one per cent of women with eclampsia die.[ medical citation needed ]
Maternal complications [edit]
A puerperal disorder or postpartum disorder is a complication which presents primarily during the puerperium, or postpartum period. The postpartum period can be divided into three distinct stages; the initial or acute phase, six to 12 hours after childbirth; subacute postpartum period, which lasts two to six weeks, and the delayed postpartum period, which can last up to six months. In the subacute postpartum period, 87% to 94% of women report at least one health problem.[116] [117] Long term health problems (persisting after the delayed postpartum period) are reported by 31 per cent of women.[118]
Postpartum bleeding [edit]
Postpartum bleeding is the leading cause of death of birthing mothers in the world, especially in the developing world. Globally it occurs about 8.7 million times and results in 44,000 to 86,000 deaths per year. Uterine atony, the inability of the uterus to contract, is the most common cause of postpartum bleeding. Following delivery of the placenta, the uterus is left with a large area of open blood vessels which must be constricted to avoid blood loss. Retained placental tissue and infection may contribute to uterine atony. Heavy blood loss leads to hypovolemic shock, insufficient perfusion of vital organs and death if not rapidly treated.[ medical citation needed ]
Postpartum infections [edit]
Postpartum infections, also known as childbed fever and puerperal fever, are any bacterial infections of the reproductive tract following childbirth or miscarriage. Signs and symptoms usually include a fever greater than 38.0 °C (100.4 °F), chills, lower abdominal pain, and possibly bad-smelling vaginal discharge. The infection usually occurs after the first 24 hours and within the first ten days following delivery. Infection remains a major cause of maternal deaths and morbidity in the developing world. The work of Ignaz Semmelweis was seminal in the pathophysiology and treatment of childbed fever and his work saved many lives.[ medical citation needed ]
Psychological complications [edit]
Childbirth can be an intense event and strong emotions, both positive and negative, can be brought to the surface. Abnormal and persistent fear of childbirth is known as tokophobia. The prevalence of fear of childbirth around the world ranges between 4–25%, with 3–7% of pregnant women having clinical fear of childbirth.[119] [120]
Most new mothers may experience mild feelings of unhappiness and worry after giving birth. Babies require a lot of care, so it is normal for mothers to be worried about, or tired from, providing that care. The feelings, often termed the "baby blues", affect up to 80 per cent of mothers. They are somewhat mild, last a week or two, and usually go away on their own.[121]
Postpartum depression is different from the "baby blues". With postpartum depression, feelings of sadness and anxiety can be extreme and might interfere with a woman's ability to care for herself or her family. Because of the severity of the symptoms, postpartum depression usually requires treatment. The condition, which occurs in nearly 15 per cent of births, may begin shortly before or any time after childbirth, but commonly begins between a week and a month after delivery.[121]
Childbirth-related posttraumatic stress disorder is a psychological disorder that can develop in women who have recently given birth.[122] [123] [124] Causes include issues such as an emergency C-section, preterm labour, inadequate care during labour, lack of social support following childbirth, and others. Examples of symptoms include intrusive symptoms, flashbacks and nightmares, as well as symptoms of avoidance (including amnesia for the whole or parts of the event), problems in developing a mother-child attachment, and others similar to those commonly experienced in posttraumatic stress disorder (PTSD). Many women who are experiencing symptoms of PTSD after childbirth are misdiagnosed with postpartum depression or adjustment disorders. These diagnoses can lead to inadequate treatment.[125]
Postpartum psychosis is a rare psychiatric emergency in which symptoms of high mood and racing thoughts (mania), depression, severe confusion, loss of inhibition, paranoia, hallucinations and delusions set in, beginning suddenly in the first two weeks after childbirth. The symptoms vary and can change quickly.[126] It usually requires hospitalisation. The most severe symptoms last from two to 12 weeks, and recovery takes six months to a year.[126]
Fetal complications [edit]

Mechanical fetal injury may be caused by improper rotation of the fetus.
Five causes make up about 80 per cent of newborn deaths globally: prematurity, low-birth-weight, infections, lack of oxygen at birth, and trauma during birth.[24]
Stillbirth [edit]
Stillbirth is typically defined as fetal death at or after 20 to 28 weeks of pregnancy.[127] [128] It results in a baby born without signs of life.[128]
Worldwide prevention of most stillbirths is possible with improved health systems.[128] [129] About half of stillbirths occur during childbirth, and stillbirth is more common in the developing than developed world.[128] Otherwise depending on how far along the pregnancy is, medications may be used to start labour or a type of surgery known as dilation and evacuation may be carried out.[130] Following a stillbirth, women are at higher risk of another one; however, most subsequent pregnancies do not have similar problems.[131]
Worldwide in 2015 there were about 2.6 million stillbirths that occurred after 28 weeks of pregnancy (about 1 for every 45 births).[128] [132] They occur most commonly in the developing world, particularly South Asia and Sub-Saharan Africa.[128] In the United States for every 167 births there is one stillbirth.[132] Stillbirth rates have declined, though more slowly since the 2000s.[133]
Preterm birth [edit]
Preterm birth is the birth of an infant at fewer than 37 weeks gestational age. It is estimated that one in 10 babies are born prematurely. Premature birth is the leading cause of death in children under five years of age though many that survive experience disabilities including learning defects and visual and hearing problems. Causes for early birth may be unknown or may be related to certain chronic conditions such as diabetes, infections, and other known causes. The World Health Organization has developed guidelines with recommendations to improve the chances of survival and health outcomes for preterm infants.[134]
Neonatal infection [edit]

Disability-adjusted life year for neonatal infections and other (perinatal) conditions per 100,000 inhabitants in 2004. Excludes prematurity and low birth weight, birth asphyxia and birth trauma which have their own maps/data.[135]
no data
less than 150
150–300
300–450
450–600
600–750
750–900
900–1050
1050–1200
1200–1350
1350–1500
1500–1850
more than 1850
Newborns are prone to infection in the first month of life. The organism S. agalactiae (Group B Streptococcus) or (GBS) is most often the cause of these occasionally fatal infections. The baby contracts the infection from the mother during labour. In 2014 it was estimated that about one in 2000 newborn babies have GBS bacterial infections within the first week of life, usually evident as respiratory disease, general sepsis, or meningitis.[136]
Untreated sexually transmitted infections (STIs) are associated with congenital and infections in newborn babies, particularly in the areas where rates of infection remain high. The majority of STIs have no symptoms or only mild symptoms that may not be recognised. Mortality rates resulting from some infections may be high, for example the overall perinatal mortality rate associated with untreated syphilis is 30 per cent.[137]
Perinatal asphyxia [edit]
Perinatal asphyxia is the medical condition resulting from deprivation of oxygen to a newborn infant that lasts long enough during the birth process to cause physical harm, usually to the brain.[138] Perinatal asphyxia or Hypoxia is one of the primary causes for birth injuries.[139] Hypoxic damage can occur to most of the infant's organs (heart, lungs, liver, gut, kidneys), but brain damage is of most concern and perhaps the least likely to quickly or completely heal.[138] Hypoxia is not a common damage during delivery, however, there are several risks factors that can lead to it; such as: vacuum or forceps delivery injury, placental abruption, among others.[139] Birth asphyxia can be prevented if healthcare providers recognize risk factors on time and take action; because if they don't oxygen depravation can lead to disabilities in the child such as: Cerebral Palsy or Autism and others that could affect the child's life for good.[140]
Mechanical fetal injury [edit]
Risk factors for fetal birth injury include fetal macrosomia (big baby), maternal obesity, the need for instrumental delivery, and an inexperienced attendant. Specific situations that can contribute to birth injury include breech presentation and shoulder dystocia. Most fetal birth injuries resolve without long term harm, but brachial plexus injury may lead to Erb's palsy or Klumpke's paralysis.[141]
History [edit]
Role of males [edit]
Historically, women have been attended and supported by other women during labour and birth. Midwife training in European cities began in the 1400s, but rural women were usually assisted by female family or friends.[142] However, it was not simply a ladies' social bonding event as some historians have portrayed—fear and pain often filled the atmosphere, as death during childbirth was a common occurrence.[143] In the United States before the 1950s, a father would not be in the birthing room. It did not matter if it was a home birth; the father would be waiting downstairs or in another room in the home. If it was in a hospital, then the father would wait in the waiting room.[144] Fathers were only permitted in the room if the life of the mother or baby was severely at-risk. In 1522, a German physician was sentenced to death for sneaking into a delivery room dressed as a woman.[142]
The majority of guidebooks related to pregnancy and childbirth were written by men who had never been involved in the birthing process.[ according to whom? ] A Greek physician, Soranus of Ephesus, wrote a book about obstetrics and gynaecology in the second century, which was referenced for the next thousand years. The book contained endless home remedies for pregnancy and childbirth, many of which would be considered heinous by modern women and medical professionals.[142]
Both preterm and full term infants benefit from skin to skin contact, sometimes called Kangaroo care, immediately following birth and for the first few weeks of life. Some fathers have begun to hold their newborns skin to skin; the new baby is familiar with the father's voice and it is believed that contact with the father helps the infant to stabilise and promotes father to infant bonding. Looking at recent studies, a 2019 review found that the level of oxytocin was found to increase not only in mothers who had experienced early skin to skin attachment with their infants but in the fathers as well, suggesting a neurobiological connection. [145] If the infant's mother had a caesarean birth, the father can hold their baby in skin-to-skin contact while the mother recovers from the anaesthetic.[146]
Hospitals [edit]
Historically, most women gave birth at home without emergency medical care available. In the early days of hospitalisation of childbirth, a 17th-century maternity ward in Paris was incredibly congested, with up to five pregnant women sharing one bed. At this hospital, one in five women died during the birthing process.[142] At the onset of the Industrial Revolution, giving birth at home became more difficult due to congested living spaces and dirty living conditions. That drove urban and lower-class women to newly-available hospitals, while wealthy and middle-class women continued to labour at home.[147] Consequently, wealthier women experienced lower maternal mortality rates than those of a lower social class.[148] Throughout the 1900s, there was an increasing availability of hospitals, and more women began going into the hospital for labour and delivery.[149] In the United States, 5% of women gave birth in hospitals in 1900. By 1930, 50% of all women and 75% of urban-dwelling women delivered in hospitals.[142] By 1960, this number increased to 96%.[143] By the 1970s, home birth rates fell to approximately 1%.[150] In the United States, the middle classes were especially receptive to the medicalisation of childbirth, which promised a safer and less painful labour.[149]
Accompanied by the shift from home to hospital was the shift from midwife to physician. Male physicians began to replace female midwives in Europe and the United States in the 1700s. The rise in status and popularity of this new position was accompanied by a drop in status for midwives. By the 1800s, affluent families were primarily calling male doctors to assist with their deliveries, and female midwives were seen as a resource for women who could not afford better care. That completely removed women from assisting in labour, as only men were eligible to become doctors at the time. Additionally, it privatised the birthing process as family members and friends were often banned from the delivery room.[ citation needed ]
There was opposition to the change from both progressive feminists and religious conservatives. The feminists were concerned about job security for a role that had traditionally been held by women. The conservatives argued that it was immoral for a woman to be exposed in such a way in front of a man. For that reason, many male obstetricians performed deliveries in dark rooms or with their patient fully covered with a drape.[ citation needed ]
Medication [edit]
The use of pain medication in labour has been a controversial issue for hundreds of years. A Scottish woman was burned at the stake in 1591 for requesting pain relief in the delivery of twins. Medication became more acceptable in 1852, when Queen Victoria used chloroform as pain relief during labour. The use of morphine and scopolamine, also known as "twilight sleep", was first used in Germany and popularised by German physicians Bernard Kronig and Karl Gauss. This concoction offered minor pain relief but mostly allowed women to completely forget the entire delivery process. Under twilight sleep, mothers were often blindfolded and restrained as they experienced the immense pain of childbirth. The cocktail came with severe side effects, such as decreased uterine contractions and altered mental state. Additionally, babies delivered with the use of childbirth drugs often experienced temporarily-ceased breathing. The feminist movement in the United States openly and actively supported the use of twilight sleep, which was introduced to the country in 1914. Some physicians, many of whom had been using painkillers for the past fifty years, including opium, cocaine, and quinine, embraced the new drug. Others were rightfully hesitant.[142]
Caesarean sections [edit]
While forceps have gone through periods of high popularity, today they are only used in approximately 10 percent of deliveries. The caesarean section (or C-section) has become the more popular solution for difficult deliveries. In 2005, one-third of babies were born via C-section. Historically, surgical delivery was a last-resort method of extracting a baby from its deceased or dying mother. There are many conflicting stories of the first successful C-section in which both mother and baby survived. It is, however, known that the procedure had been attempted for hundreds of years before it became accepted in the beginning of the twentieth century.[142]
Natural childbirth [edit]
The reemergence of "natural childbirth" began in Europe and was adopted by some in the US as early as the late 1940s. Early supporters believed that the drugs used during deliveries interfered with "happy childbirth" and could negatively impact the newborn's "emotional wellbeing". By the 1970s, the call for natural childbirth was spread nationwide, in conjunction with the second-wave of the feminist movement.[142] While it is still most common for American women to deliver in the hospital, supporters of natural birth still widely exist, especially in the UK where midwife-assisted home births have gained popularity.[150]
Maternal mortality [edit]

810 women die every day from preventable causes related to pregnancy and childbirth. 94% occur in low and lower middle-income countries.
UNFPA estimated that 303,000 women died of pregnancy or childbirth related causes in 2015.[151] These causes range from severe bleeding to obstructed labour,[152] for which there are highly effective interventions. As women have gained access to family planning and skilled birth attendants with backup emergency obstetric care, the global maternal mortality ratio has fallen from 385 maternal deaths per 100,000 live births in 1990 to 216 deaths per 100,000 live births in 2015, and many countries halved their maternal death rates in the last 10 years.[151]
1880–1930 [edit]
Since the US began recording childbirth statistics in 1915, the US has had historically poor maternal mortality rates in comparison to other developed countries. Britain started recording maternal mortality data from 1880 onward.
Outcomes for mothers in childbirth were especially poor before 1930, because of high rates of puerperal fever.[148] Until germ theory was accepted in the mid-1800s, it was assumed that puerperal fever was caused by a variety of sources, including the leakage of breast milk into the body and anxiety. Later, it was discovered that puerperal fever was transmitted by the dirty hands and tools of doctors. That was likely responsible for the high prevalence of puerperal fever.[142]
Home births facilitated by trained midwives produced the best outcomes from 1880 to 1930 in the US and Europe, whereas physician-facilitated hospital births produced the worst. The change in trend of maternal mortality can be attributed with the widespread use of sulfonamides (the first broadly effective antibacterial drugs), along with the progression of medical technology, more extensive physician training, and less medical interference with normal deliveries.[148]
Society and culture [edit]
Costs [edit]

Cost of childbirth in several countries in 2012.[153]
According to a 2013 analysis performed commissioned by the New York Times and performed by Truven Healthcare Analytics, the cost of childbirth varies dramatically by country. In the United States the average amount actually paid by insurance companies or other payers in 2012 averaged $9,775 for an uncomplicated conventional delivery and $15,041 for a caesarean birth.[ needs update ] [153] The aggregate charges of healthcare facilities for four million annual births in the United States was estimated at over $50 billion. The summed cost of prenatal care, childbirth, and newborn care came to $30,000 for a vaginal delivery and $50,000 for a caesarian section.[ citation needed ]
In the United States, childbirth hospital stays have some of the lowest ICU utilisations. Vaginal delivery with and without complicating diagnoses and caesarean section with and without comorbidities or major comorbidities account for four of the 15 types of hospital stays with low rates of ICU utilisation (where less than 20% of visits were admitted to the ICU). During stays with ICU services, approximately 20% of costs were attributable to the ICU.[154]
A 2013 study found varying costs by facility for childbirth expenses in California, varying from $3,296 to $37,227 for a vaginal birth and from $8,312 to $70,908 for a caesarean birth.[155]
Beginning in 2014, the National Institute for Health and Care Excellence began recommending that many women give birth at home under the care of a midwife rather than an obstetrician, citing lower expenses and better healthcare outcomes.[156] [157] The median cost associated with home birth was estimated to be about $1,500 vs. about $2,500 in hospital.[158]
Location [edit]
Childbirth routinely occurs in hospitals in many developed countries. Before the 20th century and in some countries to the present day, such as the Netherlands, it has more typically occurred at home.[159]
In rural and remote communities of many countries, hospitalised childbirth may not be readily available or the best option. Maternal evacuation is the predominant risk management method for assisting mothers in these communities.[160] Maternal evacuation is the process of relocating pregnant women in remote communities to deliver their babies in a nearby urban hospital setting.[160] This practice is common in Indigenous Inuit and Northern Manitoban communities in Canada as well as Australian aboriginal communities. There has been research considering the negative effects of maternal evacuation due to a lack of social support provided to these women. These negative effects include an increase in maternal newborn complications and postpartum depression, and decreased breastfeeding rates.[160]
The exact location in which childbirth takes place is an important factor in determining nationality, in particular for birth aboard aircraft and ships.
Facilities [edit]
Facilities for childbirth include:
- A labour ward, also called a delivery ward or labour and delivery, is generally a department of a hospital that focuses on providing health care to women and their children during childbirth. It is generally closely linked to the hospital's neonatal intensive care unit and/or obstetric surgery unit if present. A maternity ward or maternity unit may include facilities both for childbirth and for postpartum rest and observation of mothers in normal as well as complicated cases.
- A maternity hospital is a hospital that specialises in caring for women while they are pregnant and during childbirth and provide care for newborn babies,
- A birthing center generally presents a simulated home-like environment. Birthing centers may be located on hospital grounds or "free standing" (that is, not affiliated with a hospital).
- A home birth is usually accomplished with the assist of a midwife. Some women choose to give birth at home without any professionals present, termed an unassisted childbirth.
Associated occupations [edit]

Model of pelvis used in the beginning of the 19th century to teach technical procedures for a successful childbirth. Museum of the History of Medicine, Porto Alegre, Brazil
Different categories of birth attendants may provide support and care during pregnancy and childbirth, although there are important differences across categories based on professional training and skills, practice regulations, and the nature of care delivered. Many of these occupations are highly professionalised, but other roles exist on a less formal basis.
"Childbirth educators" are instructors who aim to teach pregnant women and their partners about the nature of pregnancy, labour signs and stages, techniques for giving birth, breastfeeding and newborn baby care. Training for this role can be found in hospital settings or through independent certifying organisations. Each organisation teaches its own curriculum and each emphasises different techniques. The Lamaze technique is one well-known example.
Doulas are assistants who support mothers during pregnancy, labour, birth, and postpartum. They are not medical attendants; rather, they provide emotional support and non-medical pain relief for women during labour. Like childbirth educators and other unlicensed assistive personnel, certification to become a doula is not compulsory, thus, anyone can call themself a doula or a childbirth educator.[ citation needed ]
Confinement nannies are individuals who are employed to provide assistance and stay with the mothers at their home after childbirth. They are usually experienced mothers who took courses on how to take care of mothers and newborn babies.[ citation needed ]
Midwives are autonomous practitioners who provide basic and emergency health care before, during and after pregnancy and childbirth, generally to women with low-risk pregnancies. Midwives are trained to assist during labour and birth, either through direct-entry or nurse-midwifery education programs. Jurisdictions where midwifery is a regulated profession will typically have a registering and disciplinary body for quality control, such as the American Midwifery Certification Board in the United States,[161] the College of Midwives of British Columbia in Canada[162] [163] or the Nursing and Midwifery Council in the United Kingdom.[164] [165]
In the past, midwifery played a crucial role in childbirth throughout most indigenous societies. Although western civilisations attempted to assimilate their birthing technologies into certain indigenous societies, like Turtle Island, and get rid of the midwifery, the National Aboriginal Council of Midwives brought back the cultural ideas and midwifery that were once associated with indigenous birthing.[166]
In jurisdictions where midwifery is not a regulated profession, traditional birth attendants, also known as traditional or lay midwives, may assist women during childbirth, although they do not typically receive formal health care education and training.
Medical doctors who practise in the field of childbirth include categorically specialised obstetricians, family practitioners and general practitioners whose training, skills and practices include obstetrics, and in some contexts general surgeons. These physicians and surgeons variously provide care across the whole spectrum of normal and abnormal births and pathological labour conditions. Categorically specialised obstetricians are qualified surgeons, so they can undertake surgical procedures relating to childbirth. Some family practitioners or general practitioners also perform obstetrical surgery. Obstetrical procedures include cesarean sections, episiotomies, and assisted delivery. Categorical specialists in obstetrics are commonly trained in both obstetrics and gynaecology (OB/GYN), and may provide other medical and surgical gynaecological care, and may incorporate more general, well-woman, primary care elements in their practices. Maternal-fetal medicine specialists are obstetrician/gynecologists subspecialised in managing and treating high-risk pregnancy and delivery.
Anaesthetists or anesthesiologists are medical doctors who specialise in pain relief and the use of drugs to facilitate surgery and other painful procedures. They may contribute to the care of a woman in labour by performing an epidural or by providing anaesthesia (often spinal anaesthesia) for Cesarean section or forceps delivery. They are experts in pain management during childbirth.
Obstetric nurses assist midwives, doctors, women, and babies before, during, and after the birth process, in the hospital system. They hold various nursing certifications and typically undergo additional obstetric training in addition to standard nursing training.
Paramedics are healthcare providers that are able to provide emergency care to both the mother and infant during and after delivery using a wide range of medications and tools on an ambulance. They are capable of delivering babies but can do very little for infants that become "stuck" and are unable to be delivered vaginally.
Lactation consultants assist the mother and newborn to breastfeed successfully. A health visitor comes to see the mother and baby at home, usually within 24 hours of discharge, and checks the infant's adaptation to extrauterine life and the mother's postpartum physiological changes.
Non-western communities [edit]
Cultural values, assumptions, and practices of pregnancy and childbirth vary across cultures. For example, some Maya women who work in agricultural fields of some rural communities will usually continue to work in a similar function to how they normally would throughout pregnancy, in some cases working until labour begins.[167]
Comfort and proximity to extended family and social support systems may be a childbirth priority of many communities in developing countries, such as the Chillihuani in Peru and the Mayan town of San Pedro La Laguna.[167] [168] Home births can help women in these cultures feel more comfortable as they are in their own home with their family around them helping out in different ways.[167] Traditionally, it has been rare in these cultures for the mother to lie down during childbirth, opting instead for standing, kneeling, or walking around prior to and during birthing.[168] [167]
Some communities rely heavily on religion for their birthing practices. It is believed that if certain acts are carried out, then it will allow the child for a healthier and happier future. One example of this is the belief in the Chillihuani that if a knife or scissors are used for cutting the umbilical cord, it will cause for the child to go through clothes very quickly. In order to prevent this, a jagged ceramic tile is used to cut the umbilical cord.[168] In Mayan societies, ceremonial gifts are presented to the mother throughout pregnancy and childbirth in order to help her into the beginning of her child's life.[167]
Ceremonies and customs can vary greatly between countries. See;
- Childbirth in Benin
- Childbirth in Ghana
- Childbirth in Haiti
- Childbirth in India
- Childbirth in Iraq
- Childbirth in Japan
- Childbirth in Mexico
- Childbirth in Nepal
- Childbirth in Sri Lanka
- Childbirth in Thailand
- Childbirth in Trinidad and Tobago
- Childbirth in Zambia
Collecting stem cells [edit]
It is currently possible to collect two types of stem cells during childbirth: amniotic stem cells and umbilical cord blood stem cells.[169] They are being studied as possible treatments of a number of conditions.[169]
Other aspects [edit]
In many countries, age is reckoned from the date of birth, and sometimes the birthday is celebrated annually. East Asian age reckoning starts newborns at "1", incrementing each Lunar New Year.
Some cultures view the placenta as a special part of birth, since it has been the child's life support for so many months. The placenta may be eaten by the newborn's family, ceremonially, for nutrition, or otherwise.[170] (Some animal mothers eat their afterbirth; this is called placentophagy.) Some birth professionals will process the placenta for consumption by postpartum mothers.[ citation needed ]
See also [edit]
References [edit]
- ^ "confinement – Definition of confinement in English by Oxford Dictionaries". Oxford Dictionaries – English.
- ^ "Confinement – meaning in the Cambridge English Dictionary". Cambridge Dictionary.
- ^ Lunze K, Bloom DE, Jamison DT, Hamer DH (January 2013). "The global burden of neonatal hypothermia: systematic review of a major challenge for newborn survival". BMC Medicine. 11 (1): 24. doi:10.1186/1741-7015-11-24. PMC3606398. PMID 23369256.
- ^ a b Martin RJ, Fanaroff AA, Walsh MC (2014). Fanaroff and Martin's Neonatal-Perinatal Medicine: Diseases of the Fetus and Infant. Elsevier Health Sciences. p. 116. ISBN978-0-323-29537-6. Archived from the original on 11 September 2017.
- ^ a b c d e f Education material for teachers of midwifery : midwifery education modules (PDF) (2nd ed.). Geneva [Switzerland]: World Health Organisation. 2008. p. 3. ISBN978-92-4-154666-9. Archived (PDF) from the original on 21 February 2015.
- ^ a b Memon HU, Handa VL (May 2013). "Vaginal childbirth and pelvic floor disorders". Women's Health. 9 (3): 265–77, quiz 276–77. doi:10.2217/whe.13.17. PMC3877300. PMID 23638782.
- ^ a b Martin E (2015). Concise Colour Medical l.p.Dictionary. Oxford University Press. p. 375. ISBN978-0-19-968799-2. Archived from the original on 11 September 2017.
- ^ a b "The World Factbook". www.cia.gov. 11 July 2016. Retrieved 30 July 2016.
- ^ "Preterm birth Fact sheet N°363". WHO. November 2015. Archived from the original on 7 March 2015. Retrieved 30 July 2016.
- ^ Buck GM, Platt RW (2011). Reproductive and perinatal epidemiology. Oxford: Oxford University Press. p. 163. ISBN978-0-19-985774-6. Archived from the original on 11 September 2017.
- ^ Co-Operation, Organisation for Economic; Development (2009). Doing better for children. Paris: OECD. p. 105. ISBN978-92-64-05934-4. Archived from the original on 11 September 2017.
- ^ Olsen O, Clausen JA (September 2012). "Planned hospital birth versus planned home birth". The Cochrane Database of Systematic Reviews (9): CD000352. doi:10.1002/14651858.CD000352.pub2. PMC4238062. PMID 22972043.
- ^ Fossard Ed, Bailey M (2016). Communication for Behavior Change: Volume lll: Using Entertainment–Education for Distance Education. Sage Publications India. ISBN978-93-5150-758-1. Archived from the original on 11 September 2017. Retrieved 31 July 2016.
- ^ a b "Birth". The Columbia Electronic Encyclopedia (6 ed.). Columbia University Press. 2016. Archived from the original on 6 March 2016. Retrieved 30 July 2016 – via Encyclopedia.com.
- ^ a b c d e f g "Pregnancy Labor and Birth". Women's Health. 27 September 2010. Archived from the original on 28 July 2016. Retrieved 31 July 2016.
The first stage begins with the onset of labour and ends when the cervix is fully opened. It is the longest stage of labour, usually lasting about 12 to 19 hours
..
The second stage involves pushing and delivery of your baby. It usually lasts 20 minutes to two hours. - ^ McDonald SJ, Middleton P, Dowswell T, Morris PS (July 2013). "Effect of timing of umbilical cord clamping of term infants on maternal and neonatal outcomes". The Cochrane Database of Systematic Reviews. 7 (7): CD004074. doi:10.1002/14651858.CD004074.pub3. PMC6544813. PMID 23843134.
- ^ a b Phillips, Raylene. "Uninterrupted Skin-to-Skin Contact Immediately After Birth". Medscape. Archived from the original on 3 April 2015. Retrieved 21 December 2014.
- ^ a b "Essential Antenatal, Perinatal and Postpartum Care" (PDF). Promoting Effective Perinatal Care. WHO. Archived (PDF) from the original on 24 September 2015. Retrieved 21 December 2014.
- ^ a b "Care of healthy women and their babies during childbirth". National Collaborating Centre for Women's and Children's Health. National Institute for Health and Care Excellence. December 2014. Archived from the original on 12 February 2015. Retrieved 21 December 2014.
- ^ Hofmeyr GJ, Hannah M, Lawrie TA (July 2015). "Planned caesarean section for term breech delivery". The Cochrane Database of Systematic Reviews (7): CD000166. doi:10.1002/14651858.CD000166.pub2. PMC6505736. PMID 26196961.
- ^ "Childbirth and beyond". womenshealth.gov. 13 December 2016. Retrieved 20 November 2018.
- ^ Childbirth: Labour, Delivery and Immediate Postpartum Care. World Health Organization. 2015. p. Chapter D. ISBN978-92-4-154935-6. Archived from the original on 11 September 2017. Retrieved 31 July 2016.
- ^ Molina G, Weiser TG, Lipsitz SR, Esquivel MM, Uribe-Leitz T, Azad T, Shah N, Semrau K, Berry WR, Gawande AA, Haynes AB (December 2015). "Relationship Between Cesarean Delivery Rate and Maternal and Neonatal Mortality". JAMA. 314 (21): 2263–70. doi:10.1001/jama.2015.15553. PMID 26624825.
- ^ a b World Health Organization. "Newborns: reducing mortality". World Health Organization. Archived from the original on 3 April 2017. Retrieved 1 February 2017.
- ^ Weber SE (January 1996). "Cultural aspects of pain in childbearing women". Journal of Obstetric, Gynecologic, and Neonatal Nursing. 25 (1): 67–72. doi:10.1111/j.1552-6909.1996.tb02515.x. PMID 8627405.
- ^ Callister LC, Khalaf I, Semenic S, Kartchner R, et al. (December 2003). "The pain of childbirth: perceptions of culturally diverse women". Pain Management Nursing. 4 (4): 145–54. doi:10.1016/S1524-9042(03)00028-6. PMID 14663792.
- ^ Hodnett ED (May 2002). "Pain and women's satisfaction with the experience of childbirth: a systematic review". American Journal of Obstetrics and Gynecology. 186 (5 Suppl Nature): S160-72. doi:10.1016/S0002-9378(02)70189-0. PMID 12011880.
- ^ Harms, Rogert W. Does back labor really happen? Archived 4 February 2016 at the Wayback Machine, mayoclinic.com, Retrieved 8 September 2014
- ^ Meyer D (2007). "Selective serotonin reuptake inhibitors and their effects on relationship satisfaction". The Family Journal. 15 (4): 392–97. doi:10.1177/1066480707305470. S2CID 144945177.
- ^ Bowen R (12 July 2010). "Oxytocin". Hypertexts for Biomedical Sciences. Archived from the original on 29 August 2014. Retrieved 18 August 2013.
- ^ Zlotnick C, Johnson SL, Miller IW, Pearlstein T, et al. (April 2001). "Postpartum depression in women receiving public assistance: pilot study of an interpersonal-therapy-oriented group intervention". The American Journal of Psychiatry. 158 (4): 638–40. doi:10.1176/appi.ajp.158.4.638. PMID 11282702.
- ^ Chabrol H, Teissedre F, Saint-Jean M, Teisseyre N, Sistac C, Michaud C, Roge B (2002). "[Detection, prevention and treatment of postpartum depression: a controlled study of 859 patients]". L'Encephale. 28 (1): 65–70. PMID 11963345.
- ^ Pillitteri A (2010). "Chapter 15: Nursing Care of a Family During Labor and Birth". Maternal & Child Health Nursing: Care of the Childbearing & Childrearing Family. Hagerstown, Maryland: Lippincott Williams & Wilkins. p. 350. ISBN978-1-58255-999-5. Archived from the original on 28 June 2014. Retrieved 18 August 2013.
- ^ Levine D (15 March 2012). "Types of Forceps Used in Delivery". Healthline. Healthline Networks. Retrieved 10 August 2013.
- ^ Goldberg AE (2 March 2018). "Cervical Ripening". Medscape . Retrieved 10 May 2018.
- ^ Kupferminc M, Lessing JB, Yaron Y, Peyser MR (December 1993). "Nifedipine versus ritodrine for suppression of preterm labour". British Journal of Obstetrics and Gynaecology. 100 (12): 1090–94. doi:10.1111/j.1471-0528.1993.tb15171.x. PMID 8297841. S2CID 24521943.
- ^ Jokic M, Guillois B, Cauquelin B, Giroux JD, Bessis JL, Morello R, Levy G, Ballet JJ (March 2000). "Fetal distress increases interleukin-6 and interleukin-8 and decreases tumour necrosis factor-alpha cord blood levels in noninfected full-term neonates". BJOG. 107 (3): 420–25. doi:10.1111/j.1471-0528.2000.tb13241.x. PMID 10740342.
- ^ Lyrenäs S, Clason I, Ulmsten U (February 2001). "In vivo controlled release of PGE2 from a vaginal insert (0.8 mm, 10 mg) during induction of labour". BJOG. 108 (2): 169–78. doi:10.1111/j.1471-0528.2001.00039.x. PMID 11236117. S2CID 45247771.
- ^ a b c d "Labor and delivery, postpartum care". Mayo Clinic . Retrieved 7 May 2018.
- ^ Novak S. "The Most Popular Time for Babies to Be Born". Washington Post. Archived from the original on 16 June 2018. Retrieved 9 May 2018.
- ^ Reiter RJ, Tan DX, Korkmaz A, Rosales-Corral SA (2013). "Melatonin and stable circadian rhythms optimize maternal, placental and fetal physiology". Human Reproduction Update. 20 (2): 293–307. doi:10.1093/humupd/dmt054. PMID 24132226.
- ^ Giacalone PL, Vignal J, Daures JP, Boulot P, Hedon B, Laffargue F (March 2000). "A randomised evaluation of two techniques of management of the third stage of labour in women at low risk of postpartum haemorrhage". BJOG. 107 (3): 396–400. doi:10.1111/j.1471-0528.2000.tb13236.x. PMID 10740337.
- ^ Hantoushzadeh S, Alhusseini N, Lebaschi AH (February 2007). "The effects of acupuncture during labour on nulliparous women: a randomised controlled trial". The Australian & New Zealand Journal of Obstetrics & Gynaecology. 47 (1): 26–30. doi:10.1111/j.1479-828X.2006.00674.x. PMID 17261096. S2CID 23495692.
- ^ Satin AJ (1 July 2013). "Latent phase of labor". UpToDate. Wolters Kluwer. Archived from the original on 3 March 2016. (subscription required)
- ^ Murray LJ, Hennen L, Scott J (2005). The BabyCenter Essential Guide to Pregnancy and Birth: Expert Advice and Real-World Wisdom from the Top Pregnancy and Parenting Resource . Emmaus, Pennsylvania: Rodale Books. pp. 294–295. ISBN978-1-59486-211-3 . Retrieved 18 August 2013.
- ^ Mayo clinic staff. "Cervical effacement and dilation". Mayo Clinic. Archived from the original on 4 December 2016. Retrieved 31 January 2017.
- ^ "WHO recommendations Intrapartum care for a positive childbirth experience (Recommendation 5)" (PDF). World Health Organization . Retrieved 6 May 2018.
- ^ Obstetric Data Definitions Issues and Rationale for Change Archived 6 November 2013 at the Wayback Machine, 2012 by ACOG.
- ^ Boyle A, Reddy UM, Landy HJ, Huang CC, Driggers RW, Laughon SK (July 2013). "Primary cesarean delivery in the United States". Obstetrics and Gynecology. 122 (1): 33–40. doi:10.1097/AOG.0b013e3182952242. PMC3713634. PMID 23743454.
- ^ "Birth (Parturition) | Boundless Anatomy and Physiology". courses.lumenlearning.com . Retrieved 26 February 2021.
- ^ "WHO recommendations Intrapartum care for a positive childbirth experience (item #3.2.2.)" (PDF). World Health Organization . Retrieved 6 May 2018.
- ^ Zhang J, Troendle JF, Yancey MK (October 2002). "Reassessing the labor curve in nulliparous women". American Journal of Obstetrics and Gynecology. 187 (4): 824–28. doi:10.1067/mob.2002.127142. PMID 12388957. Archived from the original on 18 January 2016.
- ^ "Abnormal Labour". Medscape . Retrieved 14 May 2018.
- ^ "WHO recommendations Intrapartum care for a positive childbirth experience (item #33)" (PDF). World Health Organization . Retrieved 6 May 2018.
- ^ Rouse DJ, Weiner SJ, Bloom SL, Varner MW, et al. (October 2009). "Second-stage labor duration in nulliparous women: relationship to maternal and perinatal outcomes". American Journal of Obstetrics and Gynecology. 201 (4): 357.e1–7. doi:10.1016/j.ajog.2009.08.003. PMC2768280. PMID 19788967.
- ^ Jangsten E, Mattsson LÅ, Lyckestam I, Hellström AL, et al. (February 2011). "A comparison of active management and expectant management of the third stage of labour: a Swedish randomised controlled trial". BJOG. 118 (3): 362–69. doi:10.1111/j.1471-0528.2010.02800.x. PMID 21134105.
- ^ Weeks AD (December 2008). "The retained placenta". Best Practice & Research. Clinical Obstetrics & Gynaecology. 22 (6): 1103–17. doi:10.1016/j.bpobgyn.2008.07.005. PMID 18793876.
- ^ Ball H (June 2009). "Active management of the third state of labour is rare in some developing countries". International Perspectives on Sexual and Reproductive Health. 35 (2). Archived from the original on 4 March 2016.
- ^ Stanton C, Armbruster D, Knight R, Ariawan I, et al. (March 2009). "Use of active management of the third stage of labour in seven developing countries". Bulletin of the World Health Organization. 87 (3): 207–15. doi:10.2471/BLT.08.052597. PMC2654655. PMID 19377717.
- ^ International Confederation of Midwives; International Federation of Gynaecologists Obstetricians (2004). "Joint statement: management of the third stage of labour to prevent post-partum haemorrhage". Journal of Midwifery & Women's Health. 49 (1): 76–77. doi:10.1016/j.jmwh.2003.11.005. PMID 14710151.
- ^ Mathai M, Gülmezoglu AM, Hill S (2007). WHO recommendations for the prevention of postpartum haemorrhage (PDF) (Report). Geneva: World Health Organization, Department of Making Pregnancy Safer. Archived from the original (PDF) on 5 July 2009.
- ^ McDonald SJ, Middleton P, Dowswell T, Morris PS (July 2013). McDonald SJ (ed.). "Effect of timing of umbilical cord clamping of term infants on maternal and neonatal outcomes". The Cochrane Database of Systematic Reviews. 7 (7): CD004074. doi:10.1002/14651858.CD004074.pub3. PMC6544813. PMID 23843134.
- ^ Campbell D (10 July 2013). "Hospitals warned to delay cutting umbilical cords after birth". The Guardian . Retrieved 11 June 2018.
- ^ Gjerdingen DK, Froberg DG (January 1991). "The fourth stage of labor: the health of birth mothers and adoptive mothers at six-weeks postpartum". Family Medicine. 23 (1): 29–35. PMID 2001778.
- ^ a b WHO (2013). "WHO recommendations on postnatal care of the mother and newborn". World Health Organization. Archived from the original on 22 December 2014. Retrieved 22 December 2014.
- ^ Whitaker, Amy K.; Chen, Beatrice A. (5 October 2017). "Society of Family Planning Guidelines: Postplacental insertion of intrauterine devices". Contraception (published January 2018). 97 (1): 2–13. doi:10.1016/j.contraception.2017.09.014. ISSN 0010-7824. PMID 28987293.
- ^ "Immediate Postpartum Long-Acting Reversible Contraception". www.acog.org . Retrieved 20 April 2020.
- ^ "Postpartum Assessment". ATI Nursing Education. Archived from the original on 24 December 2014. Retrieved 24 December 2014.
- ^ Mayo clinic staff. "Postpartum care: What to expect after a vaginal delivery". Mayo Clinic. Archived from the original on 21 December 2014. Retrieved 23 December 2014.
- ^ "Rooming-in: An Essential Evolution in American Maternity Care", By Jennifer Usianov. National Institute for Childre's Health Quality. {https://www.nichq.org/insight/rooming-essential-evolution-american-maternity-care} Retrieved November 1, 2021.
- ^ Saloojee H (4 January 2008). "Early skin-to-skin contact for mothers and their healthy newborn infants". The WHO Reproductive Health Library. WHO. Archived from the original on 21 December 2014. Retrieved 23 December 2014.
- ^ Crenshaw J (2007). "Care practice #6: no separation of mother and baby, with unlimited opportunities for breastfeeding". The Journal of Perinatal Education. 16 (3): 39–43. doi:10.1624/105812407X217147. PMC1948089. PMID 18566647.
- ^ Moore ER, Bergman N, Anderson GC, Medley N (November 2016). "Early skin-to-skin contact for mothers and their healthy newborn infants". The Cochrane Database of Systematic Reviews. 2016 (11): CD003519. doi:10.1002/14651858.CD003519.pub4. PMC3979156. PMID 27885658.
- ^ Mozurkewich EL, Chilimigras JL, Berman DR, Perni UC, Romero VC, King VJ, Keeton KL (October 2011). "Methods of induction of labour: a systematic review". BMC Pregnancy and Childbirth. 11: 84. doi:10.1186/1471-2393-11-84. PMC3224350. PMID 22032440.
- ^ a b "Rates for total cesarean section, primary cesarean section, and vaginal birth after cesarean (VBAC), United States, 1989–2010" (PDF). Childbirth Connection website. Relentless Rise in Cesarian Rate. August 2012. Archived from the original (PDF) on 17 February 2013. Retrieved 29 August 2013.
- ^ Main E, Oshiro B, Chagolla B, Bingham D, Dang-Kilduff L, Kowalewski L (July 2010). "Elimination of Non-medically Indicated (Elective) Deliveries Before 39 Weeks Gestational Age" (PDF). Patient Safety Council (1st ed.). March of Dimes. Archived from the original (PDF) on 20 November 2012. Retrieved 29 August 2013.
- ^ "Recent Declines in Induction of Labor by Gestational Age". Centers for Disease Control and Prevention . Retrieved 9 May 2018.
- ^ Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Mathews TJ, Kirmeyer S, Osterman MJ (August 2010). "Births: final data for 2007" (PDF). National Vital Statistics Reports : From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 58 (24): 1–85. PMID 21254725. Archived (PDF) from the original on 21 August 2013.
- ^ ACOG District II Patient Safety and Quality Improvement Committee (December 2011). "Oxytocin for Induction" (PDF). Optimizing Protocols in Obstetrics. Series 1. American Congress of Obstetricians and Gynecologists (ACOG). Archived from the original (PDF) on 21 June 2013. Retrieved 29 August 2013.
- ^ "Share of births attended by skilled health staff". Our World in Data . Retrieved 5 March 2020.
- ^ National Institute for Health and Care Excellence. "Intrapartum care: care of healthy women and their babies during childbirth". National Institute for Health and Care Excellence. Archived from the original on 18 February 2015. Retrieved 11 February 2015.
- ^ Tranmer JE, Hodnett ED, Hannah ME, Stevens BJ (2005). "The effect of unrestricted oral carbohydrate intake on labor progress". Journal of Obstetric, Gynecologic, and Neonatal Nursing. 34 (3): 319–28. doi:10.1177/0884217505276155. PMID 15890830.
- ^ O'Sullivan G, Scrutton M (March 2003). "NPO during labor. Is there any scientific validation?". Anesthesiology Clinics of North America. 21 (1): 87–98. doi:10.1016/S0889-8537(02)00029-9. PMID 12698834.
- ^ Singata M, Tranmer J, Gyte GM (August 2013). Singata M (ed.). Pregnancy and Childbirth Group. "Restricting oral fluid and food intake during labour". The Cochrane Database of Systematic Reviews. 8 (8): CD003930. doi:10.1002/14651858.CD003930.pub3. PMC4175539. PMID 23966209. Lay summary – Cochrane Summaries (22 August 2013).
- ^ Basevi V, Lavender T (November 2014). "Routine perineal shaving on admission in labour". The Cochrane Database of Systematic Reviews (11): CD001236. doi:10.1002/14651858.CD001236.pub2. PMC7076285. PMID 25398160.
- ^ Lumbiganon P, Thinkhamrop J, Thinkhamrop B, Tolosa JE (September 2014). "Vaginal chlorhexidine during labour for preventing maternal and neonatal infections (excluding Group B Streptococcal and HIV)". The Cochrane Database of Systematic Reviews. 9 (9): CD004070. doi:10.1002/14651858.CD004070.pub3. PMC7104295. PMID 25218725.
- ^ Haas, David M.; Morgan, Sarah; Contreras, Karenrose; Kimball, Savannah (26 April 2020). "Vaginal preparation with antiseptic solution before cesarean section for preventing postoperative infections". The Cochrane Database of Systematic Reviews. 4: CD007892. doi:10.1002/14651858.CD007892.pub7. ISSN 1469-493X. PMC7195184. PMID 32335895.
- ^ Liabsuetrakul, T; Choobun, T; Peeyananjarassri, K; Islam, QM (26 March 2020). "Antibiotic prophylaxis for operative vaginal delivery". The Cochrane Database of Systematic Reviews. 2020 (3): CD004455. doi:10.1002/14651858.CD004455.pub5. PMC7096725. PMID 32215906.
- ^ "Forceps or vacuum delivery". NHS . Retrieved 15 November 2020.
- ^ Jones L, Othman M, Dowswell T, Alfirevic Z, Gates S, Newburn M, Jordan S, Lavender T, Neilson JP (March 2012). "Pain management for women in labour: an overview of systematic reviews". The Cochrane Database of Systematic Reviews. 3 (3): CD009234. doi:10.1002/14651858.CD009234.pub2. PMC7132546. PMID 22419342.
- ^ American Academy of Pediatrics Committee on Fetus Newborn; American College of Obstetricians Gynecologists Committee on Obstetric Practice (April 2014). "Immersion in water during labor and delivery". Pediatrics. 133 (4): 758–61. doi:10.1542/peds.2013-3794. PMID 24652300.
- ^ Bohren MA, Hofmeyr GJ, Sakala C, Fukuzawa RK, Cuthbert A (July 2017). "Continuous support for women during childbirth". The Cochrane Database of Systematic Reviews. 7 (8): CD003766. doi:10.1002/14651858.CD003766.pub6. PMC6483123. PMID 28681500.
- ^ Caughey AB, Cahill AG, Guise JM, Rouse DJ (March 2014). "Safe prevention of the primary cesarean delivery". American Journal of Obstetrics and Gynecology. 210 (3): 179–93. doi:10.1016/j.ajog.2014.01.026. PMID 24565430.
- ^ Lancashire, Liz (9 July 2018). "Medicine Administration for Midwives". Norfolk and Norwich University Hospitals . Retrieved 16 June 2019.
- ^ Kumar, Manoj; Paes, Bosco (July 2003). "Epidural Opioid Analgesia and Neonatal Respiratory Depression". Journal of Perinatology. 23 (5): 425–27. doi:10.1038/sj.jp.7210905. ISSN 1476-5543. PMID 12847541.
- ^ Thorp JA, Breedlove G (June 1996). "Epidural analgesia in labor: an evaluation of risks and benefits". Birth. 23 (2): 63–83. doi:10.1111/j.1523-536X.1996.tb00833.x. PMID 8826170.
- ^ a b Anim-Somuah M, Smyth RM, Cyna AM, Cuthbert A (May 2018). "Epidural versus non-epidural or no analgesia for pain management in labour". The Cochrane Database of Systematic Reviews. 2018 (5): CD000331. doi:10.1002/14651858.CD000331.pub4. PMC6494646. PMID 29781504.
- ^ Alehagen S, Wijma B, Lundberg U, Wijma K (September 2005). "Fear, pain and stress hormones during childbirth". Journal of Psychosomatic Obstetrics and Gynaecology. 26 (3): 153–65. doi:10.1080/01443610400023072. PMID 16295513. S2CID 44646591.
- ^ Loftus JR, Hill H, Cohen SE (August 1995). "Placental transfer and neonatal effects of epidural sufentanil and fentanyl administered with bupivacaine during labor". Anesthesiology. 83 (2): 300–08. doi:10.1097/00000542-199508000-00010. PMID 7631952.
- ^ Wei SQ, Luo ZC, Xu H, Fraser WD (September 2009). "The effect of early oxytocin augmentation in labor: a meta-analysis". Obstetrics and Gynecology. 114 (3): 641–49. doi:10.1097/AOG.0b013e3181b11cb8. PMID 19701046. S2CID 29571476.
- ^ "Recommendations for Augmentation of Labour" (PDF). World Health Organization . Retrieved 9 May 2018.
- ^ Jiang H, Qian X, Carroli G, Garner P (February 2017). "Selective versus routine use of episiotomy for vaginal birth". The Cochrane Database of Systematic Reviews. 2017 (2): CD000081. doi:10.1002/14651858.CD000081.pub3. PMC5449575. PMID 28176333.
- ^ Bastos, Maria Helena; Furuta, Marie; Small, Rhonda; McKenzie-McHarg, Kirstie; Bick, Debra (10 April 2015). "Debriefing interventions for the prevention of psychological trauma in women following childbirth". The Cochrane Database of Systematic Reviews (4): CD007194. doi:10.1002/14651858.CD007194.pub2. ISSN 1469-493X. PMID 25858181.
- ^ Vernon D (6 February 2007). "Men At Birth – Should Your Bloke Be There?". BellyBelly.com.au. Archived from the original on 1 June 2013. Retrieved 23 August 2013.
- ^ Bohren, MA; Hofmeyr, GJ; Sakala, C; Fukuzawa, RK; Cuthbert, A (6 July 2017). "Continuous support for women during childbirth". The Cochrane Database of Systematic Reviews. 7 (8): CD003766. doi:10.1002/14651858.CD003766.pub6. PMC6483123. PMID 28681500.
- ^ Hammond P, Johnson A (1986). "Tocodynamometer". In Brown M (ed.). The Medical Equipment Dictionary. London: Chapman & Hall. ISBN978-0-412-28290-4. Archived from the original on 4 March 2016. Retrieved 23 August 2013. Online version accessed.
- ^ Alfirevic, Zarko; Gyte, Gillian ML; Cuthbert, Anna; Devane, Declan (2017). "Continuous cardiotocography (CTG) as a form of electronic fetal monitoring (EFM) for fetal assessment during labour". Cochrane Database of Systematic Reviews. 2 (5): CD006066. doi:10.1002/14651858.CD006066.pub3. PMC6464257. PMID 28157275. Retrieved 6 May 2018.
- ^ "WHO recommendations Intrapartum care for a positive childbirth experience (Recommendation 17)" (PDF). World Health Organization . Retrieved 7 May 2018.
- ^ a b "Mortality and Burden of Disease Estimates for WHO Member States in 2004" (xls). Department of Measurement and Health Information, World Health Organization. Archived from the original on 2 February 2014.
- ^ "Maternal health". United Nations Population Fund . Retrieved 24 April 2018.
- ^ Van Lerberghe W, De Brouwere V (2001). "Of Blind Alleys and Things That Have Worked: History's Lessons on Reducing Maternal Mortality" (PDF). In De Brouwere V, Van Lerberghe W (eds.). Safe Motherhood Strategies: A Review of the Evidence. Studies in Health Services Organisation and Policy. 17. Antwerp: ITG Press. pp. 7–33. ISBN978-90-76070-19-3.
Where nothing effective is done to avert maternal death, "natural" mortality is probably of the order of magnitude of 1,500/100,000.
- ^ Propublica, Nina Martin; Montagne, Renee (12 May 2017). "U.S. Has The Worst Rate Of Maternal Deaths In The Developed World". NPR . Retrieved 25 April 2018.
- ^ "Severe Complications for Women During Childbirth Are Skyrocketing – and Could Often Be Prevented". ProPublica. 22 December 2017. Retrieved 4 May 2018.
- ^ Levi J, Kohn D, Johnson K (June 2011). "Healthy Women, Healthy Babies: How health reform can improve the health of women and babies in America" (PDF). Washington, D.C.: Trust for America's Health. Archived (PDF) from the original on 24 June 2012. Retrieved 29 August 2013.
- ^ Education material for teachers of midwifery : midwifery education modules (PDF) (2nd ed.). Geneva: World Health Organisation. 2008. pp. 38–44. ISBN978-9241546669. Archived (PDF) from the original on 21 February 2015.
- ^ Glazener CM, Abdalla M, Stroud P, Naji S, Templeton A, Russell IT (April 1995). "Postnatal maternal morbidity: extent, causes, prevention and treatment". British Journal of Obstetrics and Gynaecology. 102 (4): 282–87. doi:10.1111/j.1471-0528.1995.tb09132.x. PMID 7612509. S2CID 38872754.
- ^ Thompson JF, Roberts CL, Currie M, Ellwood DA (June 2002). "Prevalence and persistence of health problems after childbirth: associations with parity and method of birth". Birth. 29 (2): 83–94. doi:10.1046/j.1523-536X.2002.00167.x. PMID 12051189.
- ^ Borders N (2006). "After the afterbirth: a critical review of postpartum health relative to method of delivery". Journal of Midwifery & Women's Health. 51 (4): 242–48. doi:10.1016/j.jmwh.2005.10.014. PMID 16814217.
- ^ Jaju S, Al Kharusi L, Gowri V (2015). "Antenatal prevalence of fear associated with childbirth and depressed mood in primigravid women". Indian Journal of Psychiatry. 57 (2): 158–61. doi:10.4103/0019-5545.158152. PMC4462784. PMID 26124521.
- ^ Lukasse M, Schei B, Ryding EL (October 2014). "Prevalence and associated factors of fear of childbirth in six European countries". Sexual & Reproductive Healthcare. 5 (3): 99–106. doi:10.1016/j.srhc.2014.06.007. hdl:10642/2246. PMID 25200969.
- ^ a b "Postpartum Depression Facts". National Institute of Mental Health . Retrieved 4 May 2018.
- ^ Lapp LK, Agbokou C, Peretti CS, Ferreri F (September 2010). "Management of post traumatic stress disorder after childbirth: a review". Journal of Psychosomatic Obstetrics and Gynaecology. 31 (3): 113–22. doi:10.3109/0167482X.2010.503330. PMID 20653342. S2CID 23594561.
- ^ Condon J (February 2010). "Women's mental health: a "wish-list" for the DSM V". Archives of Women's Mental Health. 13 (1): 5–10. doi:10.1007/s00737-009-0114-1. PMID 20127444. S2CID 1102994.
- ^ Martin C (2012). Perinatal Mental Health : a Clinical Guide. Cumbria England: M & K Pub. p. 26. ISBN978-1907830495.
- ^ Alder J, Stadlmayr W, Tschudin S, Bitzer J (June 2006). "Post-traumatic symptoms after childbirth: what should we offer?". Journal of Psychosomatic Obstetrics and Gynaecology. 27 (2): 107–12. doi:10.1080/01674820600714632. PMID 16808085. S2CID 21859634.
- ^ a b Jones I, Chandra PS, Dazzan P, Howard LM (November 2014). "Bipolar disorder, affective psychosis, and schizophrenia in pregnancy and the post-partum period". Lancet. 384 (9956): 1789–99. doi:10.1016/S0140-6736(14)61278-2. PMID 25455249. S2CID 44481055.
- ^ "Stillbirth: Overview". NICHD. 23 September 2014. Archived from the original on 5 October 2016. Retrieved 4 October 2016.
- ^ a b c d e f "Stillbirths". World Health Organization. Archived from the original on 2 October 2016. Retrieved 29 September 2016.
- ^ "Ending preventable stillbirths An Executive Summary for The Lancet's Series" (PDF). The Lancet. January 2016. Archived from the original (PDF) on 12 July 2018. Retrieved 31 January 2020.
- ^ "How do health care providers manage stillbirth?". NICHD. 23 September 2014. Archived from the original on 5 October 2016. Retrieved 4 October 2016.
- ^ "Stillbirth: Other FAQs". NICHD. 23 September 2014. Archived from the original on 5 October 2016. Retrieved 4 October 2016.
- ^ a b "How common is stillbirth?". NICHD. 23 September 2014. Archived from the original on 5 October 2016. Retrieved 4 October 2016.
- ^ Draper, Elizabeth S.; Manktelow, Bradley N.; Smith, Lucy; Rubayet, Sayed; Hirst, Jane; Neuman, Melissa; King, Carina; Osrin, David; Prost, Audrey (6 February 2016). "Stillbirths: rates, risk factors, and acceleration towards 2030". The Lancet. 387 (10018): 587–603. doi:10.1016/S0140-6736(15)00837-5. ISSN 0140-6736. PMID 26794078.
- ^ "Preterm Birth". World Health Organization . Retrieved 26 April 2018.
- ^ "Mortality and Burden of Disease Estimates for WHO Member States in 2004" (xls). Department of Measurement and Health Information, World Health Organization. February 2009.
- ^ Ohlsson A, Shah VS (June 2014). "Intrapartum antibiotics for known maternal Group B streptococcal colonization". The Cochrane Database of Systematic Reviews (6): CD007467. doi:10.1002/14651858.CD007467.pub4. PMID 24915629.
- ^ "Sexually transmitted infections (STIs)". World Health Organization. May 2013. Archived from the original on 25 November 2014. Retrieved 30 August 2013.
- ^ a b van Handel M, Swaab H, de Vries LS, Jongmans MJ (July 2007). "Long-term cognitive and behavioral consequences of neonatal encephalopathy following perinatal asphyxia: a review". European Journal of Pediatrics. 166 (7): 645–54. doi:10.1007/s00431-007-0437-8. PMC1914268. PMID 17426984.
- ^ a b "How Anoxia and Hypoxia at Birth Affects Your Baby". Birth Injury Guide . Retrieved 22 October 2021.
- ^ "The Insider's Guide To Oxygen Deprivation At Birth". Birth Injury Guide . Retrieved 22 October 2021.
- ^ Warwick R, Williams PL, eds. (1973). Gray's Anatomy (35th British ed.). London: Longman. p. 1046. ISBN978-0443010118.
- ^ a b c d e f g h i Hutter Epstein, M.D., Randi (2011). Get Me Out: A History of Childbirth from the Garden of Eden to the Sperm Bank. New York: W.W. Norton & Company, Inc.
- ^ a b Dye NS (Autumn 1980). "History of Childbirth in America". Signs: Journal of Women in Culture and Society. The University of Chicago Press. 6 (1): 97–108. doi:10.1086/493779. JSTOR 3173968. PMID 21213655. S2CID 144068193.
- ^ Leavitt, Judith W. (1988). Brought to Bed: Childbearing in America, 1750–1950. University of Oxford. pp. 90–91. ISBN978-0-19-505690-7.
- ^ Scatliffe, N.; Casavant, S.; Vittner, D.; Cong, X. (2019). "Oxytocin and early parent-infant interactions: A systematic review". International Journal of Nursing Sciences. 6 (4): 445–453. doi:10.1016/j.ijnss.2019.09.009. PMC6838998. PMID 31728399.
- ^ "Fathers and skin-to-skin contact". Kangaroo Mother Care. Retrieved 30 April 2013.
- ^ Cassidy T (2006). Birth. New York: Atlantic Monthly Press. pp. 54–55. ISBN978-0-87113-938-2.
- ^ a b c Loudon I (July 2000). "Maternal mortality in the past and its relevance to developing countries today". The American Journal of Clinical Nutrition. 72 (1 Suppl): 241S–246S. doi:10.1093/ajcn/72.1.241S. PMID 10871589.
- ^ a b Thompson CJ (2005). "Consumer Risk Perceptions in a Community of Reflexive Doubt". Journal of Consumer Research. 32 (2): 235–48. doi:10.1086/432233.
- ^ a b A natural process? Women, men and the medicalisation of childbirth". broughttolife.sciencemuseum.org.uk. Retrieved 3 December 2018.
- ^ a b "Maternal health". United Nations Population Fund. Retrieved 29 January 2017.
- ^ GBD 2013 Mortality Causes of Death Collaborators (January 2015). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC4340604. PMID 25530442.
- ^ a b Rosenthal E (30 June 2013). "American Way of Birth, Costliest in the World". The New York Times. Archived from the original on 1 January 2017.
- ^ Barrett ML, Smith MW, Elizhauser A, Honigman LS, Pines JM (December 2014). "Utilization of Intensive Care Services, 2011". HCUP Statistical Brief #185. Rockville, MD: Agency for Healthcare Research and Quality. Archived from the original on 2 April 2015.
- ^ Hsia RY, Akosa Antwi Y, Weber E (January 2014). "Analysis of variation in charges and prices paid for vaginal and caesarean section births: a cross-sectional study". BMJ Open. 4 (1): e004017. doi:10.1136/bmjopen-2013-004017. PMC3902513. PMID 24435892.

- ^ National Collaborating Centre for Women's and Children's Health (2007). Intrapartum Care: Care of Healthy Women and Their Babies During Childbirth. NICE Clinical Guidelines, No. 55. London: RCOG. ISBN9781904752363. PMID 21250397. [ page needed ]
- ^ "Recommendations: Intrapartum care for healthy women and babies". National Institute for Health and Care Excellence. National Institute for Health and Care Excellence. Retrieved 6 December 2020.
- ^ Bennhold K, Louis CS (3 December 2014). "British Regulator Urges Home Births Over Hospitals for Uncomplicated Pregnancies - NYTimes.com". The New York Times. Archived from the original on 28 March 2017.
- ^ Stearns PN, ed. (1993). Encyclopedia of Social History. Garland Reference Library of Social Sciences. V. 780. London: Taylor & Francis. p. 144. ISBN978-0-8153-0342-8. Archived from the original on 2 January 2016.
- ^ a b c Tait HN, Cidro J (2018). Indigenous experiences of pregnancy and birth. ISBN978-1772581355. OCLC 1012401274.
- ^ "About AMCB". Archived from the original on 23 February 2014. Retrieved 20 February 2014.
- ^ "Welcome to the College of Midwives of British Columbia". College of Midwives of British Columbia website. Archived from the original on 17 September 2013. Retrieved 30 August 2013.
- ^ Province of British Columbia (21 August 2013) [Revised Statues of British Columbia 1996]. "Health Professions Act". Statues and Regulations of British Columbia internet version. Vancouver, British Columbia, Canada: Queens Printer. Archived from the original on 25 August 2013. Retrieved 30 August 2013.
- ^ "Our role". Nursing & Midwifery Council website. London, England. 31 August 2011 [Created 2010-02-24]. Archived from the original on 5 September 2013. Retrieved 30 August 2013.
- ^ "The Nursing and Midwifery Order 2001". London, England: Her Majesty's Stationery Office, The National Archives, Ministry of Justice, Her Majesty's Government. 2002. Archived from the original on 8 August 2013.
- ^ Burton N (2015). Natal signs : cultural representations of pregnancy, birth and parenting. Demeter Press. ISBN978-1926452326. OCLC 949328683.
- ^ a b c d e Barbara R (2011). Developing destinies : a Mayan midwife and town. Oxford University Press. ISBN978-0-19-531990-3. OCLC 779676136. [ page needed ]
- ^ a b c Inge B (2006). Growing up in a culture of respect child rearing in highland Peru. University of Texas Press. OCLC 748863692. [ page needed ]
- ^ a b Dziadosz M, Basch RS, Young BK (March 2016). "Human amniotic fluid: a source of stem cells for possible therapeutic use". American Journal of Obstetrics and Gynecology. 214 (3): 321–27. doi:10.1016/j.ajog.2015.12.061. PMID 26767797.
- ^ Vernon DM, ed. (2005). Having a Great Birth in Australia: Twenty Stories of Triumph, Power, Love and Delight from the Women and Men who Brought New Life Into the World. Canberra, Australia: Australian College of Midwives. p. 56. ISBN978-0-9751674-3-4.
External links [edit]
![]() 17-pound baby born in Russia at Wikinews
17-pound baby born in Russia at Wikinews
- Spontaneous Vaginal Delivery, Video by Merck Manual Professional Edition
- [1] Maternal Morbidity/Mortality in the Media
| Classification | D
|
|---|
Letters to Baby While in Waiting Room During Labor
Source: https://en.wikipedia.org/wiki/Childbirth
0 Response to "Letters to Baby While in Waiting Room During Labor"
Post a Comment